Most management retirees have been covered by the UnitedHealth Care Group Medicare Advantage plan since January of 2014. As a result of the recent union contract, our understanding is that our union brothers and sister retirees, who will be Medicare eligible, will be under the same plan effective January 1, 2017.
Consequently, we thought it would be prudent to survey our members about their experiences with the plan. During and after the survey, there was some criticism that sufficient space was not allowed for extra commentary so I have now provided my own email address for members to comment. For those who have no access to email, please know that you are invited to write to me at the Association offices.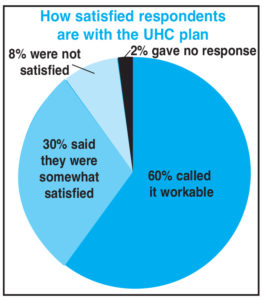
According to a May 2016 report from the Kaiser Family Foundation, 31%, or 17.6 million, of beneficiaries on Medicare have Medicare Advantage Plan coverage and that number has increased in virtually all states.
Of the 17.6 million, virtually all enroll as individuals. About 3.2 million are in a group plan, as my wife and I are.
Medicare pays the insurer (UHC) a fixed payment in effect making UHC a “contractor” to Medicare, for which they are compensated. I mention this because that compensation has become controversial due to provisions of the Affordable Care Act that will reduce that compensation in 2017. That reduction will make the Medicare subsidy more in line with that which is provided by Medicare to the average beneficiary. It will still be higher, but perhaps not high enough to satisfy corporate greed.
Right now the Medicare compensation is higher for beneficiaries of Medicare Advantage plans. The employer, and often the retiree too, pay a premium for any additional benefits or lower cost sharing. That premium, paid by Verizon and us, may rise in 2017 to fill the gap caused by the decrease in subsidy.
Our member survey showed that 85 percent of almost 2,000 members were covered by this plan. A very small number of respondents (28 people) indicated that they had dropped out for various reasons, the largest being that providers would not take the insurance. Other reasons were out-of-pocket costs due to a particular negative event. Thirteen people said that they are no longer covered by a Verizon health plan. Other results indicated that:
1) Almost 86% said their providers accept the Group Medicare Advantage Plan for routine visits.
2) Just over 18% had to change some providers who refused to accept.
3) During a recent hospital stay 518 members, or 33% of those responding, indicated that the plan had been accepted.
4) Interestingly, 24 respondents said they paid a significant amount of money for hospitalizations that were not covered.
When asked how satisfied people were with the coverage from this plan, 60% called it workable and said they were very satisfied. Almost 30% claimed they were “somewhat satisfied” and about 8% were not satisfied at all. When asked if a test that had been requested by a Primary Care Provider had been denied authorization, 14% answered “yes.”
Common complaints related to me in the emails included:
- The frustration associated with denial of service. So many specialists from orthopedists and dermatologists to special labs refused services regardless of whether they also take Medicare patients.
- Many were annoyed that Primary Care Providers (PCPs) or specialists would often order tests only to be told that the decision was vetoed by UHC. A two-pager is provided by UHC to give to providers who resist. Frequently, that is enough. However, very often it is not enough. Both Verizon and UHC will be adamant that if the provider takes Medicare, they should take the plan. Unfortunately, that does not always happen.
- Very low compensation to providers as well as extreme delays in processing were other common threads from the emails. I suspect that is more a problem with Medicare than with UHC. However, our plan is a “Managed Care” plan and that does make a difference regarding acceptability, according to some physicians. When you dispute a claim finding, you deal with Medicare, not UHC. I know from this personal experience.
- Feedback indicated nostalgia for past coverage, which included something that was truly “supplemental.” The reality is that you cannot have a “Medigap” plan when you have a Medicare Advantage Plan. However, MA plans do include prescription drug coverage so . you don’t need to invest in Part D.
For our union brothers and sisters who are getting into this plan on Jan. 1, 2017, I urge you to spend the time now checking with your providers and local hospitals to make sure they accept it. If it is a medical group or hospital, make sure all of their participating physicians and specialists and labs also accept the plan. You don’t want to schedule surgery at a hospital that accepts the insurance only to find out that the anesthesiologist does not.
Generally, when traveling, if you require emergency medical attention, you will probably not be denied. However, be prepared that there may be an issue with admittance and treatment costs. In June of this year Kaiser put out a complete report on Medicare Advantage Hospital Networks and how much they vary throughout the nation.
The results of this survey and our findings will be shared with the human resources leadership of Verizon. Whether or not this results in any positive change is anybody’s guess, but they should know of our experiences and reactions.